BACKGROUND: Essential thrombocythemia (ET) and polycythemia vera (PV) are BCR::ABL1 negative myeloproliferative neoplasms (MPNs) characterized by overproduction of one or more mature myeloid cell lineages and high thrombotic risk. Diabetes mellitus (DM) is a rare cardiovascular (CV) comorbidity in MPNs and the optimal treatment target levels of glycated hemoglobin (HbA1c) in MPNs remain unknown.
OBJECTIVE&METHODS: This multicenter study was conducted in Croatia and Serbia in the period between 01/1997 and 01/23 and investigated clinical correlations of HbA1c in ET and PV patients whose diagnoses were reassessed according to 2016 WHO criteria. We retrospectively collected data regarding diabetic ET and PV patients with available HbA1c at disease diagnosis, stratified them according to HbA1c levels, and compared their clinical outcomes to a control group of 93 non-diabetic ET and PV patients. Outcomes of interest were time to thrombosis (TTT; death as a censoring event) and overall survival (OS). Survival analyses were based on Kaplan-Meier method and performed with log-rank test and the Cox-regression analysis. The study was approved by Ethics Committees from all participating centers.
RESULTS: We included 109 MPN patients (33 ET and 76 PV) with DM (all type II); median age was 69 years (range 37-86), 60 (55%) were females, 81 (74.3%) were JAK2- and 10 (9.2%) CALR-positive. Ninety-two (84.4%) patients were classified as high-risk (age>60 years or prior thrombosis), 68 (62.4%) received hydroxyurea (HU), 91 (83.5%) had arterial hypertension, 44 (40.4%) hyperlipidemia, and 36 (33%) were smokers. The median follow-up time was 38 months; 16 (14.7%) thrombotic (13 arterial and 3 venous) events and 25 deaths (22.9%) occured during this time.
Median HbA1c in diabetic MPN patients was 6.8% (range 4.8-16.2%). There were no associations of HbA1c with disease phenotype, age, sex, mutational status, prior thrombosis, presence of individual CV risk factors, or any of the blood cell count components (p>0.050 for all analyses).
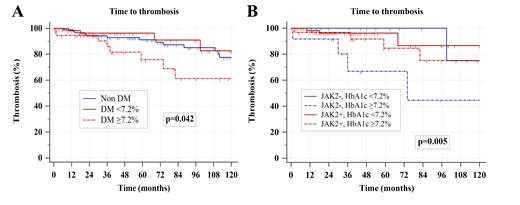
ROC curve defined the optimal HbA1c cut-off level of ≥7.2% for the best discrimination of thrombotic events in MPN patients with DM. Diabetic MPN patients with low HbA1c (<7.2%) had similar TTT (median 182 months) as non-diabetic MPN patients (median 197 months) whereas those with higher HbA1c (≥7.2%) had significantly worse TTT (median 124 months; HR 3.76, p=0.012), as presented in Figure 1A. The detrimental effect of high HbA1c was evident in high-risk (HR 3.2, p=0.031) but not in low-risk diabetic MPN patients (p=0.115). Also, JAK2-negative diabetic MPN patients with higher HbA1c had inferior TTT when compared to their counterparts (HR 28.17, p<0.001), with no difference among JAK2-positive patients (Figure 1B). There were significant interactions between high HbA1c, thrombotic risk, and advanced age (p=0.026), higher leukocytes (p=0.028), higher erythrocytes (p=0.007), higher platelets (p=0.034), higher hematocrit (p=0.007) and higher hemoglobin (p=0.013), with older age and higher blood counts favoring higher thrombotic risk associated with high HbA1c. There was no difference in OS when comparing non-diabetic to diabetic MPN patients with respect to HbA1c (p=0.209).
In the multivariate Cox regression model, high HbA1c (HR 5.04, p=0.013) remained as the only variable associated with inferior TTT among diabetic MPN patients when additionally controlling for age, sex, history of thrombosis, presence of JAK2 mutation, HU treatment, baseline leukocyte counts, and the presence of at least one other CV risk factor.
DISCUSSION: This study demonstrated that diabetic MPN patients with low (<7.2%) HbA1c had similar TTT as non-diabetic patients suggesting that stringent control of DM in MPNs is extremely important; this effect was most evident in JAK2-negative diabetic MPN patients. Also, significant interactions with high trombotic risk were found between high HbA1c, older age, and different myeloid cell lineages, suggesting that uncontrolled DM acts synergistically with MPN clone and underlies CV development. However, no correlations between HbA1c and blood cell counts were detected, indicating that HbA1c measurements may not be accurrate in MPNs for DM diagnosis. The lack of association of high HbA1c with OS is probably related to optimal post-thrombotic management. Future studies are needed to elucidate optimal HbA1c values for the diagnosis and treatment of DM in MPNs.
Disclosures
No relevant conflicts of interest to declare.